When considering ageing and mental health, it would not be surprising to regard ageing as a risk factor for mental health in itself. However, this is a misnomer. Research has consistently demonstrated that mental health issues improve as one ages. A community-based study of 1546 adults aged 21-100 year found, via a structured multi-cohort investigation, an accelerated deterioration in physical and cognitive functioning, averaging 1.5 to 2 standard deviations over the adult lifespan. In contrast, there was a linear improvement (of about 1 standard deviation) in mental health attributes over the same life period. (Thomas M et al, 2016). A study of 40000 people found that age alone had a protective effect on mental health symptoms, and found that this effect increased from 1994 to 2007 (2.5% to 17.3%) (Lorem G et al, 2017). In Australia, results of the Australian Bureau of Statistics 2007 National Survey of Mental Health and Wellbeing revealed that adults aged 75–85 years with mental health needs reported some of the lowest rates of mental health service use, compared to other age groups (Slade et al, 2007). Similar findings have been noted for the US, Canada and the UK (Wuthrich et al, 2015).
This suggests that, for older adults, one of the issues that potentially prevent them from receiving optimal care is in fact the assumption that mental illness is a normal part of the ageing process (Sarkisian et al, 2003). It is naturally critical that one must additionally consider the role of health care clinicians, and what their perspectives of ageing must be. Does a clinician in contact with an older person regard their mental health issues as significant? Or could a latent bias interfere with their receiving appropriate, comprehensive care?
The above should not lead one to assume that older people have a universally lower level of mental health comorbidity. Apart from dementia, there is another dimension that warrants special consideration – that of suicide. Despite the general reduction in prevalence of all mental health issues – including depression – there is a paradoxical rise in suicide with ageing. (Shah A, 2012). The Australian Bureau of Statistics identified in 2015 that Australian men aged over 85 had the highest suicide rate in Australia. Notably, this is not a uniquely Australian phenomenon, present in the US, Singapore, China, the UK, but not in Japan – a possibly culturally-bound omission. Suicide in the older person suffers from being complicated with the euthanasia debate, and has been described as potentially rational.
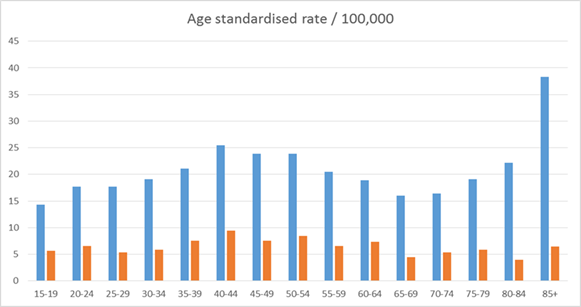
Figure: Age standardised rate of suicide attempts, against age demographics. Blue: Male, Orange: Female
The apparent legitimacy of suicide in the elderly has made some authors comment that it may be the result of a rational decision. “Frailty, dependence on others, loss of a partner, and loneliness… suicide can be interpreted as a legitimate exit in case of dramatic changes in social status and role.” In addition, ageist perspectives have considered that depression may be regarded as a normal process for the older person, and “advanced age as the antecedent of an anticipated and definitive ending. Accumulation of physical illnesses and disabilities, life events, and losses can be seen as the so-called right cause to step out of this stage of life. This interpretation—the ultimate corollary of senectus ipsa morbus—overlaps with the idea of elderly people being overwhelmed by their emotions, and seeing suicide as their only escape from an unbearable situation.” (Leo D, 2017)
Suicide – bound in concepts of identity and role – is importantly considered with another condition which is indeed ageing-related, and has been called the commonest mental illness, even if it does not have a specific disease code in any generally accepted classificatory system (Mushtaq R, 2014). A study in 2002 of coroner’s file reports of suicides in 1994 to 1998 was undertaken to understand understand more clearly the precipitant causes of suicide in an older population. Of 210 elderly people who killed themselves, 160 (76%) were clearly depressed, including a majority of the 24% deemed to have understandable reasons for suicide. Physical ill‐health or disability was the major factor leading to suicide in 34% and appeared to contribute to suicidal ideation in another 24% of those who died; it was additionally noted that they had usually not been seen by psychiatrists. (Snowdon, 2002)
Loneliness
Loneliness has been identified as being present in up to a third of older persons (AARP, 2018). Loneliness in ageing has been considered by psychoanalysts to be a result of self-inflicted narcissistic injury, in people who refuse help until very elderly, and are unable to acquire adequate adaptation to ageing. (Cohen, 1982). This viewpoint, however, is not evidence based, and primarily the result of psychoanalytic theory – which, as Cohen has noted, is itself at risk of significantly ageist attitudes. It has been associated with poorer cognitive function among older adults (Shankar A, 2013), and increased risk of several physical and mental health conditions – including cardiac disease, depression, and overall mortality. (Cacioppo J, 2018).
If one considers the older person as supposed to have improving mental health as one progresses, and yet there are remarkable elevations in suicide and loneliness, the issue of social supports necessarily is raised. And, as has been identified, one of the few consistent factors as one grows older is an increasing dependence on health care professions, which make up an incrementally relevant component of an older person’s support network.
This brings us back to the role of the clinician, and the attitude of the health care professional towards the older person. It does suggest that impact of clinicians on the older person may be more far-reaching than previously described. In the twilight of one’s life, when one is at their most vulnerable, the impact of the health-worker cannot be understated.
References:
AARP 2018. National Poll on Healthy Aging. www.healthyagingpoll.org, accessed 21/11/19
Cacioppo JT and Cacioppo S. The growing problem of loneliness. Lancet 2018;391(10119):426.
Cohen, N.A. (1982). On Loneliness and the Ageing Process. Int. J. Psycho-Anal., 63:149-155.
Leo D (2017) Ageism and suicide prevention. The Lancet, November 22, 2017
Lorem GF, Schirmer H, Wang CEA, et al(2017). Ageing and mental health: changes in self-reported health due to physical illness and mental health status with consecutive cross-sectional analysesBMJ Open 2017;7:e013629. doi: 10.1136/bmjopen-2016-013629
Mushtaq R (2014) Relationship Between Loneliness, Psychiatric Disorders and Physical Health ? A Review on the Psychological Aspects of Loneliness. Journal of Clinical and Diagnostic Research, 2014 Sep 8(9)
Sarkisian, C. A., Lee-Henderson, M. H., & Mangione, C. M. (2003). Do depressed older adults who attribute depression to “old age” believe it is important to seek care? Journal of General Internal Medicine, 18(12), 1001–1005.
Shah, A (2012) Suicide rates: age-associated trends and their correlates. Journal of Injury and Violence 4(2): 79-86
Shankar A (2013), Social Isolation and Loneliness: Relationships With Cognitive Function During 4 Years of Follow-up in the English Longitudinal Study of Ageing. Psychosomatic Medicine: February/March 2013 – Volume 75 – Issue 2 – p 161–170
Snowdon J, Baume P. (2002) A study of suicides of older people in Sydney. International Journal of Geriatric Psychiatry, 13 March
(Published in MindCafe August 2020)
